In the ever-evolving landscape of modern medicine, Deep Brain Stimulation (DBS) stands as a testament to human ingenuity and scientific advancement. This groundbreaking therapeutic approach, which might sound like something straight out of science fiction, has transformed the lives of countless patients suffering from debilitating neurological conditions. But what exactly happens when surgeons implant electrodes deep within the human brain, and how has this revolutionary treatment evolved over the decades?
At its core, DBS operates on a deceptively simple principle: the delivery of carefully controlled electrical impulses to specific regions of the brain. Yet, the elegant simplicity of this concept belies the intricate complexity of its implementation. Picture, if you will, a neural orchestra where each section plays slightly out of tune – DBS acts as the conductor, restoring harmony to the discordant symphony of misfiring neurons. This metaphor, while poetic, barely scratches the surface of the sophisticated interplay between technology and human physiology.
The remarkable journey of DBS from experimental therapy to standard treatment option spans decades of painstaking research. Neuroscientists discovered that certain brain circuits, when disrupted, could cause a cascade of symptoms ranging from uncontrollable tremors to severe depression. The breakthrough came with the realization that these circuits could be modulated – essentially “reset” – through precisely targeted electrical stimulation. This discovery opened up entirely new avenues for treating previously intractable neurological conditions.
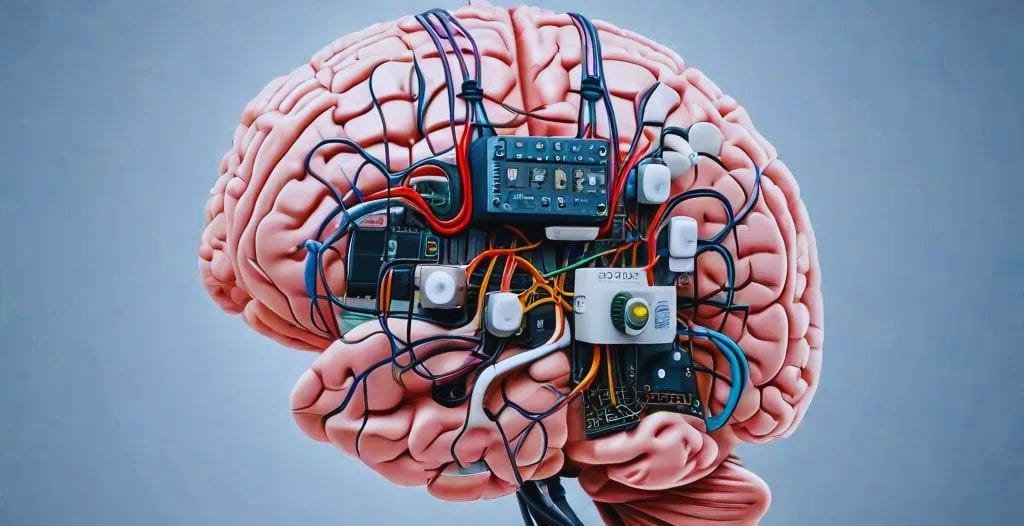
Modern DBS systems consist of three primary components: electrodes implanted in specific brain regions, a neurostimulator (often called a pulse generator) typically placed in the chest, and connecting wires that run under the skin. Think of it as a highly sophisticated pacemaker for the brain, continuously monitoring and adjusting its output to maintain optimal neural function. The level of engineering precision required to create these devices is nothing short of extraordinary.

The surgical procedure itself requires exceptional precision and expertise. Using advanced imaging techniques and stereotactic navigation systems, surgeons must thread hair-thin electrodes through the brain with sub-millimeter accuracy. One slight deviation could mean the difference between therapeutic success and failure. The patient typically remains awake during crucial portions of the surgery, allowing doctors to fine-tune the electrode placement based on real-time feedback – a process that can be both fascinating and unnerving for medical professionals and patients alike.
What makes DBS particularly fascinating is its remarkable adaptability. The same basic technology can treat an impressive array of conditions: Parkinson’s disease, essential tremor, dystonia, and even psychiatric conditions like obsessive-compulsive disorder and treatment-resistant depression. Each application requires its own unique “neural target” and stimulation parameters, showcasing the remarkable versatility of this therapeutic approach. This adaptability has led researchers to explore its potential in treating everything from chronic pain to eating disorders.
The mechanisms behind DBS’s effectiveness continue to intrigue researchers and challenge our understanding of brain function. While early theories suggested it simply inhibited overactive brain regions, current understanding points to a more nuanced picture. DBS appears to reset pathological neural patterns, restore normal brain rhythms, and promote neuroplasticity – the brain’s ability to reorganize and heal itself. This complex interplay of effects helps explain why the treatment can be effective for such a diverse range of conditions.
Recent technological advances have ushered in a new era of “smart” DBS systems. These devices can detect subtle changes in brain activity and automatically adjust stimulation parameters in real-time, much like a thermostat regulating temperature. This closed-loop approach promises even more precise and personalized treatment options for patients. Some systems can even learn from individual patient responses, gradually optimizing their performance over time.
Despite its proven track record, DBS isn’t without risks or limitations. The brain, our most complex organ, doesn’t always respond predictably to electrical stimulation. Some patients experience side effects ranging from speech difficulties to mood changes, though these can often be managed through careful programming adjustments. The challenge lies in finding the perfect balance between therapeutic benefit and potential side effects – a delicate dance that requires expertise and patience.

The economic impact of DBS technology cannot be overlooked. While the initial cost of the procedure and device is substantial, studies have shown that successful DBS treatment can significantly reduce long-term healthcare costs for many patients. This cost-benefit analysis becomes particularly relevant when considering the improved quality of life and reduced need for ongoing medical interventions that many patients experience.
The future of DBS looks increasingly bright, with researchers exploring new applications and refinements. Miniaturized components, improved battery life, and more sophisticated programming algorithms are just the beginning. Some scientists envision DBS systems that can be controlled through thought alone, while others work on combining DBS with other therapeutic approaches for enhanced effectiveness. The potential integration with artificial intelligence and machine learning algorithms promises to make these systems even more responsive and personalized.
Conclusion
Deep Brain Stimulation represents one of neuroscience’s most remarkable achievements – a testament to our growing ability to interact with and modulate the brain’s complex circuitry. As our understanding of neural networks deepens and technology continues to advance, DBS will likely evolve into an even more powerful tool in our therapeutic arsenal. The journey from its inception to current applications demonstrates the incredible potential of combining scientific insight with technological innovation, offering hope to those affected by neurological and psychiatric conditions that were once considered untreatable.
Frequently Asked Questions
How long does a DBS device last?
The neurostimulator’s battery typically lasts 3-5 years, though newer rechargeable systems can last up to 15 years. When the battery depletes, the pulse generator requires surgical replacement, though the brain electrodes usually remain in place. The decision between rechargeable and non-rechargeable systems depends on factors like patient preference, device usage patterns, and specific medical requirements.
Is the patient awake during DBS surgery?
Yes, patients are typically awake during crucial parts of the procedure to provide feedback, helping ensure optimal electrode placement. However, they receive local anesthesia and feel no pain during the surgery. This “awake” portion is essential for testing the effectiveness of electrode positioning and making real-time adjustments. The beginning and end of the surgery are performed under general anesthesia for patient comfort.
Can DBS cure neurological conditions?
DBS doesn’t cure underlying conditions but rather manages symptoms effectively. It’s important to understand that it’s a treatment option, not a cure, though it can dramatically improve quality of life for many patients. The degree of improvement varies among individuals and conditions, with some patients experiencing dramatic benefits while others may have more modest improvements.
Who is eligible for DBS?
Eligibility varies by condition and individual circumstances. Generally, candidates must have a confirmed diagnosis, have tried standard treatments without adequate success, and be in good enough health to undergo surgery. A thorough evaluation by a specialized medical team determines suitability. Factors like age, cognitive function, and overall health status are carefully considered in the selection process.
Does insurance cover DBS?
Many insurance providers, including Medicare, cover DBS for approved conditions like Parkinson’s disease and essential tremor. Coverage for newer applications may vary, and prior authorization is typically required. The coverage process often involves detailed documentation of medical necessity and previous treatment attempts.
What is the recovery period like after DBS surgery?
Recovery typically takes several weeks to months. The initial healing period focuses on surgical site recovery, while the subsequent weeks involve programming sessions to optimize the device settings. Patients usually can return to normal activities gradually, with full recovery often achieved within 3-6 months.
How often does the DBS system need adjustment?
Initial programming begins a few weeks after surgery, with frequent adjustments during the first 3-6 months. After that, adjustments are typically needed every 3-12 months, though this varies by individual. Some newer systems allow for remote adjustment, reducing the need for in-person visits.
What lifestyle changes are necessary with DBS?
While DBS allows most patients to lead relatively normal lives, certain precautions are necessary. These include avoiding strong electromagnetic fields, informing medical professionals about the implant before procedures, and carrying a medical ID card. Some activities may need modification, but most patients can resume their regular routines.
Can DBS be reversed or removed?
Yes, DBS is reversible, and the system can be turned off or removed if necessary. This reversibility is one of its key advantages over other surgical treatments. However, removal is rarely needed unless complications occur or a different treatment approach is chosen.
What are the latest developments in DBS technology?
Recent advances include directional leads allowing more precise stimulation, rechargeable batteries with longer life spans, MRI-compatible systems, and closed-loop devices that adjust stimulation based on brain activity. Researchers are also exploring new applications and combining DBS with other therapies for enhanced effectiveness.

